Abbas RazaDr. Pakistan
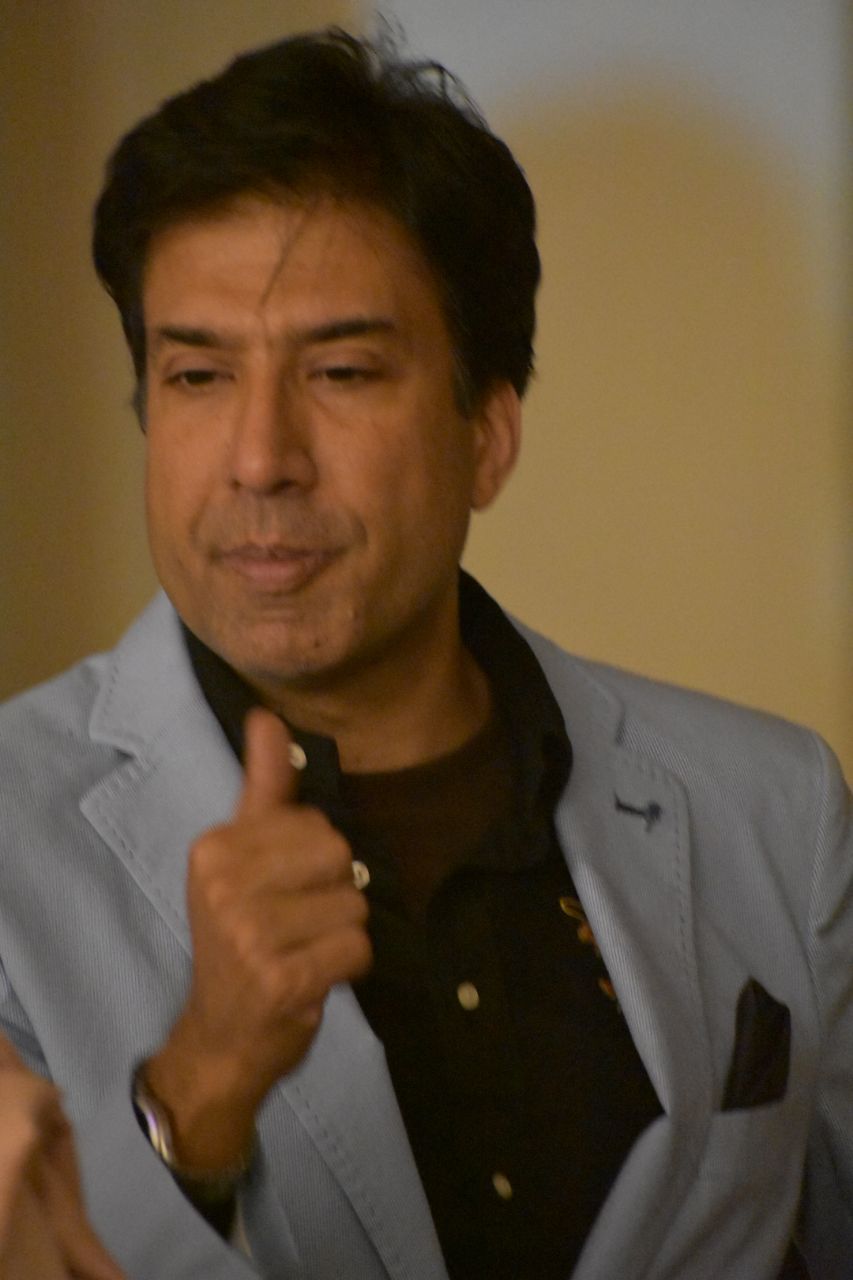
Dr. S. Abbas Raza is working as consultant Diabetologist /Endocrinologist at Shaukat Khanum Cancer Hospital & Research Center and National Hospital in Lahore, Pakistan. Dr. Raza graduated from Allama Iqbal Medical College, Lahore Pakistan. He received his Internal Medicine residency training from Atlantic City Medical Center, New Jersey, USA and also, served as Chief medical resident at the same institution. His fellowship training for Diabetes, Endocrinology and Metabolism was at University of Wisconsin, Madison, U.S.A. He is Diplomat American Board of Internal Medicine and Diplomat American Board of Diabetes, Endocrinology & Metabolism.
Government of Pakistan and President has awarded Dr. Raza with Tamgha-e-Imtiaz for his services in field of Medicine in 2022-23. It is one the highest civil award bestowed to recognize individual’s meritorious contribution to the national interests of Pakistan with significant public endeavors. He is also bestowed the honor of Global - Laureate Awards by the Endocrine Society - 2025 International Excellence in Endocrinology Award, which is considered one of the most prestigious award in Endocrine Community across globe.
Dr. Raza has been honored with Fellowship by American College of Endocrinology and Sri Lanka College of Endocrinologists. Dr. Raza has many research / scientific articles to his credit which are published in peer reviewed journals and have authored chapters in Endocrine books. He is actively involved in formulating / publication of guidelines and consensus statement for Southeast Asia region related to Diabetes and Endocrinology. Dr. Raza has also served as Chief Investigator for several national and International clinical trials.
Dr. Abbas Raza is CEO of MED (Medicine – Endocrinology and Diabetes) Consultant and involved in many projects for capacity building of physicians and outreach program for patient suffering from Endocrine disorders.
Dr. Abbas Raza currently holds the office of past President of the International Society of Endocrinology (ISE). He has also served as President of organizations including South Asian Federation of Endocrine Societies (SAFES) / Pakistan Endocrine Society (PES) and American Association of Clinical Endocrinologist (AACE) – Pakistan Chapter. SAFES includes Endocrine Societies of Afghanistan, Bangladesh, India, Maldives, Nepal, Pakistan and Sri Lanka. Pakistan Endocrine Society honored Dr. Raza with “Lifetime Achievement award”, where he serves as Executive Member since 2004.
Dr. Raza Innovation in Diabetes management include his “Dream Diabetes” project. This project takes Diabetes management to doorstep of underprivileged population suffering from Diabetes. This caters to needs of patient living in underdeveloped areas and do not have access to specialist care.
Dr. Raza also holds responsibility of Director of organizations like “Friend Of Mayo” (FOM) and Dilawar Hussain Foundation (DHF). FOM has taken responsibility of upgrading Mayo Hospital, which is a century old hospital, with inpatient - bed capacity of more than 2400 patients. This hospital caters for poor / non affording patients. While Dilawar Hussain Foundation, is a social welfare & charity organization formed in 2011, serving in the field of health, education, and community awareness. DHF runs Charity Diabetes Clinics and caters to thousands of patient suffering with Diabetes and unable to afford treatment.
21 MARCH
| Time | Session |
|---|---|
|
08:30
10:00
|
New Development in Dyslipidemia Management
Jun-Sing WangTaiwan
Moderator
Continuous Glucose Monitoring (CGM) in Asia: Behavior Change, Physician Workflow, and New Care Models
101
|
22 MARCH
| Time | Session |
|---|---|
|
11:00
12:30
|
Perspectives on Obesity in Asia-Oceania
Kathryn TanHong Kong, China
Moderator
Lipoprotein(a): What Endocrinologists Need to KnowLipoprotein(a) [Lp(a)] is a cholesterol-rich LDL-like particle with apolipoprotein(a) covalently linked to apolipoprotein B100 via a disulfide bond. Lp(a) is synthesized within the liver and there is a general inverse correlation between Lp(a) isoform size and plasma Lp(a) concentrations. About 90% of plasma Lp(a) concentration is genetically determined and plasma levels can modestly rise after menopause in women, and in conditions like hypothyroidism, nephrotic syndrome. It has been shown that elevated Lp(a) is an independent risk factor for atherosclerotic cardiovascular disease (ASCVD) and calcific aortic valve stenosis. Although Lp(a) concentration does vary with ethnicity, relationships between Lp(a) concentration and ASCVD risk remain similar across different ethnic groups. Elevated Lp(a) is considered a cardiovascular risk-enhancing or amplification factor, and recent guidelines and consensus have increasingly recommended universal screening for Lp(a). There are as yet, no approved therapies for elevated Lp(a). Current management focuses on intensifying control of concurrent risk factors, particularly LDL-C, to reduce ASCVD risk. Amongst existing lipid-lowering drugs, only proprotein convertase subtilisin/kexin type 9 inhibitors can lower Lp(a) levels modestly. Emerging RNA-based and small-molecule therapeutics are under development and are showing promising Lp(a)-lowering effects up to 80-90%. Ongoing phase 3 cardiovascular outcomes trials will determine whether effectively lowering Lp(a) can translate to cardiovascular benefit.
101
|
|
14:00
15:30
|
101
|
